Formations that occur on the skin, mucous membranes of the external and internal genital organs due to the presence of the human papillomavirus in the body are called condylomas. The surface of these neoplasms is lined with stratified squamous epithelium.

Содержание:
Features of neoplasms
Vulvar warts are growths on the external genital organs, consisting of a pathologically overgrown epithelial layer. The peculiarity of the papillomavirus is that, while in the body, it may not manifest itself for a long time.
For example, after infection, the first clinical signs may appear after 2-3 months or after several years. The main reason for the activation of the virus is the weakening of the body’s immune defenses.
Types of formations
Outwardly, warts resemble warts, the area of one lesion can reach 3 cm. Growths can occur in any part of the vulva.
Condylomas can be divided into 2 main types :
- Exophytic or pointed – visually look like elevations above the surface of the cone-shaped epithelium. They have a pinkish or flesh color. At first, a single outgrowth appears, then in the process of development whole groups are formed that merge with each other. A characteristic feature is that condylomas in the group are almost the same size. The place of localization of genital warts is the vulva, cervix, urethra.
- Endophytic or wide e – clearly differ from pointed neoplasms, as they have a wide flat base. In this case, the lesion itself does not protrude from the outside, but grows inside the tissues. Although when the lesions merge, the picture resembles genital warts. As a rule, wide condylomas are observed in the vaginal region, after a while they can spread inward, provoking the development of malignant processes in the cervix. The main danger is that a routine gynecological examination is not always able to detect such neoplasms. In addition, the appearance and growth of endophytic warts is a clear indicator of secondary syphilis.
Causes
The main route of transmission of papillomavirus is sexual. Of course, you can get infected by household means, but it is extremely rare. This is due to the fact that for the spread of the virus through household contact, several factors must be present at the same time: a decrease in immunity, insufficient hygiene, a living pathogenic microorganism in the external environment.

In contrast, sexual contact creates an optimal environment for the virus:
- humidity;
- friction;
- microtrauma;
- The pathogen enters the skin, while it does not need to survive in the external environment.
Even protected sexual contact does not guarantee the absence of infection. For example, if one of the partners has a neoplasm on the pubis or on the root of the penis, it cannot be covered with any condom. Thus, a healthy person is infected.
Provoking factors
As mentioned above, HPV can be in a latent state for a long time. The following circumstances can provoke the growth of genital warts:
- weakening of the immune system;
- various chronic diseases;
- irregular sleep and wakefulness;
- abuse of unhealthy food;
- other sexual infections;
- microcracks or injury to places of usual localization;
- disruptions in the endocrine system;
- hypothermia / overheating;
- restrictive clothing that rubs the body.
It happens that the growth of genital warts is associated with the use of contraceptives. For example, a drug taken by Yarina without a hormone test can cause a hormonal surge. That is, improperly selected drugs weaken the body, provoking the activation of HPV.
Why are genital warts dangerous?
Genital warts are dangerous because they are easily transmitted to a sexual partner. Moreover, endophytic formations contain the causative agent of syphilis in large quantities, and even protected sex can cause infection.
Pointed formations in this regard are not so dangerous. Infection occurs only during the release of the virus to the surface of the skin, in other periods the risk of transmission is minimal. On the other hand, a man may be the primary source of infection for a woman who has genital warts. Therefore, both partners should be tested.
Most often, the development and growth of genital warts of the vulva occurs in combination with inflammatory processes in the pelvic organs, for example, inflammation of the ovaries, fallopian tubes, endometrium, urethra , bladder.
Very often, these diseases have a chronic course and implicit symptoms, so specialists do not prescribe a number of necessary drugs. In 9 out of 10 cases, vulvar condylomas are diagnosed along with ureaplasma, mycoplasma, chlamydia, candidal lesions, herpes, cytomegalovirus infection, and vaginal dysbacteriosis.
Diagnosis and symptoms
As mentioned above, doctors distinguish 2 types of vulvar warts – pointed and wide. Symptoms of such neoplasms are as follows:
- on the skin or mucous membranes of the genital organs, growths of a single or multiple nature are observed, resembling cauliflower;
- a woman is tormented by constant itching and burning sensation;
- profuse discharge from the vagina, including the intermenstrual period, sometimes with streaks of pus, which indicates the presence of secondary foci of infection;
- painful feeling during sex, which is caused by injury to the neoplasm.
Diagnosis of condylomatosis includes the following activities:
- Standard examination on a gynecological chair . This method is the simplest. However, with the help of mirrors, only shallow and clearly distinguishable formations can be seen.
- Colposcopy is a more sophisticated method using magnifying glasses. To identify hidden genital warts, the doctor can treat the intended localization site with special means.
- Oncocytology is a method that includes scraping from the cervix. In the future, the material is examined for the presence of atypical cells.
- Biopsy – taking a tissue sample for examination in the laboratory. Allows to identify oncological processes.
- PCR analysis – this method allows you to determine papillomavirus in a swab taken.

Methods for the treatment of condylomatosis
Small or single condylomas can be eliminated by conservative methods. This avoids surgical intervention and, as a result, residual scars. Treatment with drugs takes a long time, but, as practice shows, it brings long-term results. Therapy is carried out by 2 groups of funds.
The action of these funds is based on suppressing the activity of the virus and strengthening the cell walls, that is, the pathogen is simply not able to penetrate inside:
- Isoprinosine/Groprinosin : Taken 3 times a day for 2-4 weeks.
- Epigen spray : applied to the vulva up to 4 times a day until the formations disappear.
- Aldara / Keravort : cream applied to the affected areas, used until the symptoms disappear completely.
- Panavir gel/spray . It is used for application until the complete disappearance of formations.
The appointment of any drug should be made by a doctor, because side reactions are possible, which will be much more difficult to cope with.
Use of immunostimulants
The funds taken by the courses, their action is aimed at restoring the body’s immune defenses. These include:
- Immunal : take 4 times a day. The course is 14–28 days.
- Polyoxidonium : suppositories – inserted into the vagina at night, course – 10 suppositories.
- Reaferon : a powder that dissolves in water and is taken 30 minutes before meals. Course – 10 days.
Methods of radical removal
You can remove warts in the following ways:
- Laser – painless and quick recovery after surgery. The operation does not take long.
- Cryodestruction is a method in which the formation is frozen with liquid nitrogen. The procedure is painless and does not require anesthesia.
- Chemically aggressive acids . They cause the death of the formation cells, while the condyloma simply disappears. The method is effective, but dangerous – contact with the reagents on the skin can cause serious burns.
- Electrocoagulation . To remove, use a special electric knife. Anesthesia is required for the operation. Possible complications in the form of scarring.
- Radio wave removal . Excision of neoplasms is performed with a radio knife, damaged vessels are cauterized. The operation is highly effective, there are practically no side effects. However, the demand for such procedures is low due to the high cost.
- Radical removal with a scalpel . It is used only when identifying large neoplasms that cannot be removed by other less traumatic methods. The operation is performed under anesthesia and is accompanied by suturing.

After the operation, a woman may experience discomfort (itching and burning) for several days. If after this period they remain, you should consult a doctor in order to prevent complications. For example, a white coating may indicate the addition of a secondary infection.
Complications
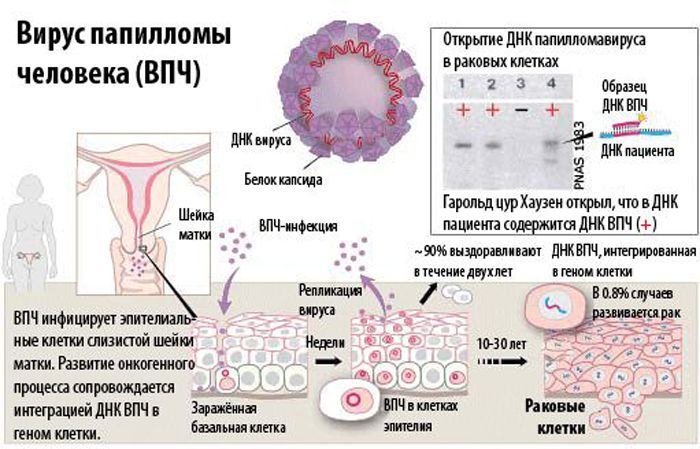
The main danger of genital warts is the possibility of their degeneration into a malignant tumor. Moreover, no additional factors are required for malignancy; in the absence of treatment, everything happens gradually. The most oncogenic strains of the human papillomavirus are 6, 11, 16 and 18. Malignancy begins with erosion and inflammation.
Even if the formation is benign, it can grow to colossal proportions, giving the owner a lot of uncomfortable sensations. Sexual intercourse becomes impossible, and simple walking causes pain. A woman develops psychological complexes.
Vulvar warts during pregnancy can cause infection of the fetus and disrupt the natural process of childbirth. Therefore, with large areas of damage, a caesarean section is prescribed.
How to prevent a relapse
Despite successful treatment, there is always a risk of recurrence. This is due to the fact that the human papillomavirus, having once entered the body, remains there until the end of a person’s days. That is, the disease is considered incurable today.
To prevent the re-growth of genital warts, it is recommended to strengthen the immune system, not to overcool or overheat. Nutrition should be balanced and include all the necessary nutrients. Avoid fatty, salty and spicy foods. It is necessary to avoid stressful situations and strong psycho-emotional experiences.
Condylomatosis is a rather dangerous disease that can degenerate into an oncological disease. To avoid dangerous consequences, you should visit a gynecologist at least 2 times a year. When the first neoplasms are detected, treatment should be started immediately, this will facilitate therapy and help avoid complications.








Мне знакомая врач-гинеколог говорила, что при проблемах с впч и его проявлениями хорошо себя зарекомендовал Аллокин альфа. Если болезнь не запущена, удаления может и не понадобиться, препарат сам справляется. Странно, что его не упомянули в статье.