Genital warts or genital warts is an infectious disease that provokes the human papillomavirus. The infection is characterized by a long course in a chronic form with periodic relapses.
The disease is considered highly contagious, especially in the acute period. The disease is quite widespread and has no sexual gradation, but there is evidence that this disease is more common in women, especially in those who are sexually active.

Содержание:
- 1 Causes of the appearance of genital warts in intimate places
- 2 Methods of infection
- 3 Risk factors
- 4 Varieties of genital warts, how they look (photo)
- 5 Places of localization in women and men
- 6 Symptoms
- 7 Diagnostic measures
- 8 Treatment of condylomatosis
- 9 Folk remedies
- 10 Why they are dangerous, complications and prognosis
- 11 Prevention measures
Causes of the appearance of genital warts in intimate places
Genital genital warts most often appear as a result of previous genital infections or with a frequent change of sexual partner. In the female half of humanity, condylomas occur when the immune system is weakened in the postpartum period or with vaginal dysbacteriosis.
According to statistics, in men who are sexually active, candidiasis causes one or more pathogenic strains of the virus. Their active reproduction leads to the appearance of characteristic formations in intimate places, however, the occurrence of genital warts in men is possible only when the body cannot resist the infectious process. If the immune system is strong enough, it will suppress the manifestations of the virus, and prevent its reproduction.
Thus, most people can be latent carriers of the virus for a long time, and signs of the presence of condylomatosis appear in them only with a decrease in immunity. Also find out how warts appear on the penis , diagnosis and treatment of the disease.
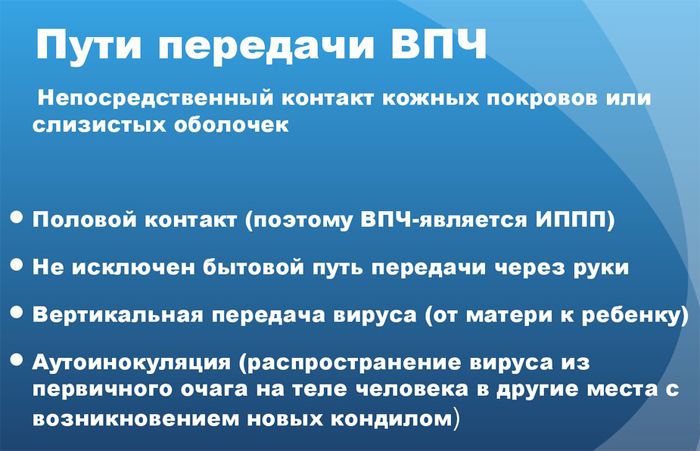
Methods of infection
Genital warts can be transmitted through sexual and domestic contact. The most common way of transmission of the virus is sexual, this is due to the peculiarity of the virus, for which constant heat, moisture and friction are considered favorable conditions. As a result of sexual contact, these conditions arise, which are comfortable for the active reproduction of the virus.
During intimacy, microtrauma of the mucous membranes is possible, through which the virus can enter the human body, and even if the immune system attacks the infection, it continues to be in the body in a dormant state and waits for favorable conditions suitable for it.
The contact-household way is less widespread, but it still exists. The papillomavirus can be found in human secretions, and if in a family all its members use the same towel and other intimate hygiene items, then the virus can be transmitted from an infected person to everyone else, including children.
As a rule, the appearance of genital warts after infection can be observed after a couple of months, however, the latent period of a viral infection can last up to a year.
Risk factors
Risk factors for women:
- weak immunity;
- frequent stress and emotional overload;
- taking antibacterial agents;
- the presence of chronic pathologies of an infectious nature;
- a combination of the presence of the papillomavirus and sexually transmitted infections – fungi, chlamydia, gonorrhea;
- frequent promiscuity;
- bad habits;
- lack of a balanced diet;
- pregnancy and lactation;
- abortions.
As for the risk factors for men, they are as follows:
- bad habits;
- immune pathologies;
- taking hormonal drugs;
- avitaminosis;
- insufficient amount of sleep;
- prolonged regular overwork;
- hypothermia or hyperthermia.
Flat warts often occur in the second stage of syphilis, such formations can appear not only on the scrotum and anus, but also in the armpits and rectum.
Important! Pathetic growths cannot disappear on their own, and because of the possible risk of their transformation into a malignant process, treatment should begin immediately upon detection.
Varieties of genital warts, how they look (photo)
Benign genital neoplasms are classified as follows:
- Genital warts – exophytic – grow outward, respectively, they are located on the skin.
- Flat warts – endophytic – grow inward, that is, they penetrate into the deep subcutaneous layers. It is these warts that have a high oncogenic index, which means they can provoke oncology. In addition, the danger lies also in the fact that it is more difficult to detect them than spiky ones.
When it comes to genital warts, most often it is genital warts that are meant, but there are other types:
- Papular – the shape of such warts resembles a dome, the color is dark red, the surface is smooth.
- Keratonic – more common in the pubic region, on the foreskin or on the penis itself. These warts have a stalk.
- Giant condylomas – look like separate patches of skin, can secrete an unpleasantly smelling secret.
- Endourethral – develop mainly near the urethra.
- Wide – such formations only outwardly resemble warts, in fact they are not a consequence of the papillomavirus – they are caused by syphilis.







Places of localization in women and men
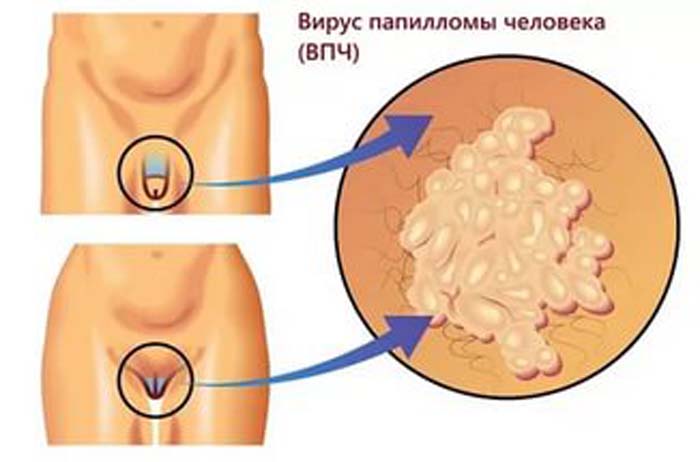
Anogenital warts can be located:
- in women – in the perianal region, at the entrance to the urethra, on the external genitalia;
- in men – in the perianal region, on the foreskin, on the glans penis .
Flat warts can be found:
- in women – on the cervix, on the vaginal mucosa. I must say that such formations can cause cervical erosion;
- in men – in the urethra, on the penis, on the foreskin.
In some cases, which are much less common, genital warts can affect the mucous membranes of the mouth, lips, bronchi and esophagus.
Symptoms
There are usually no obvious signs of genital warts, and the infected person is unaware of the problem. With the appearance of growths, discomfort occurs, since neoplasms can be injured, bleed and become inflamed.
At the same time, pain, discharge and an unpleasant odor may occur in the area of \u200b\u200btheir localization. When genital warts grow too large, they can interfere with normal sexual intercourse. Also find out what indirect signs will help you identify HPV.
In addition, the virus can manifest itself in the following non-specific symptoms:
- weakness;
- increased irritability;
- fast fatiguability;
- frequent headaches;
- in some cases, the temperature may rise.
In women, condylomatosis has more specific symptoms:
- unpleasant smell from intimate places;
- constant feeling of moisture in the vagina;
- pain in the lower abdomen;
- sensations of a foreign body in the area of the wart;
- irritation that occurs when the build-up comes into contact with underwear.
In men, with the growth of condylomas, the following can be observed:
- discomfort during urination;
- discomfort during physical exertion and walking;
- pain during intimacy;
- if the neoplasms are localized around the anus, bloody impurities in the feces can be observed;
- pain in the lower abdomen of a moderate nature.
Diagnostic measures
As a rule, the clinical picture is enough to establish a diagnosis, but the patient must still undergo the necessary studies:
- donate blood for syphilis and HIV;
- do a biopsy of the neoplasm;
- make an immunogram;
- if condylomas are located on the cervix or in the vagina, colposcopy and biomaterial sampling will be required;
- make oncocytology from the surface of growths;
- donate blood for PCR.

In the presence of typical warts, it is not necessary to determine the strain that provoked them, but since in some cases genital warts can be signs of other ailments, their presence must be excluded.
Treatment of condylomatosis
Self-treatment of neoplasms in intimate places is not only ineffective, but also quite dangerous. Given the fact that some genital warts can give impetus to the development of cancer, all therapeutic measures should be carried out under the supervision of the attending physician.
Unfortunately, it is impossible to get rid of the papillomavirus , because, having entered the body once, it remains there forever, but it is possible to reduce the risk of recurrence of its manifestation.
As soon as suspicious warts are detected, it is urgent to consult a doctor so that he can conduct all the necessary research and exclude the presence of atypical cells in the neoplasms.
Further, the growths are to be removed, only the doctor can determine the most optimal way to eliminate the wart:
- laser removal;
- radio wave method;
- cryodestruction;
- electrocoagulation.
Laser wart removal is quite simple. The tissues of the neoplasm are evaporated, which guarantees the absence of bleeding and damage to healthy areas of the mucosa. This method can remove warts of any size. After removal, a small crust remains on the mucous membrane, which disappears after a while, leaving clean skin in its place.

The radio wave method of removing genital warts is a progressive and most modern way to get rid of pathological growths. This method avoids bleeding, which means infection of the growth. After the procedure, which lasts only 10 minutes, the patient almost never has complications in the form of an inflammatory process.
Liquid nitrogen for warts removal is another effective and modern method. Under the influence of low temperature nitrogen, the protein structure of the neoplasm is destroyed, and the wart disappears. Cryodestruction is indicated for the elimination of small warts.

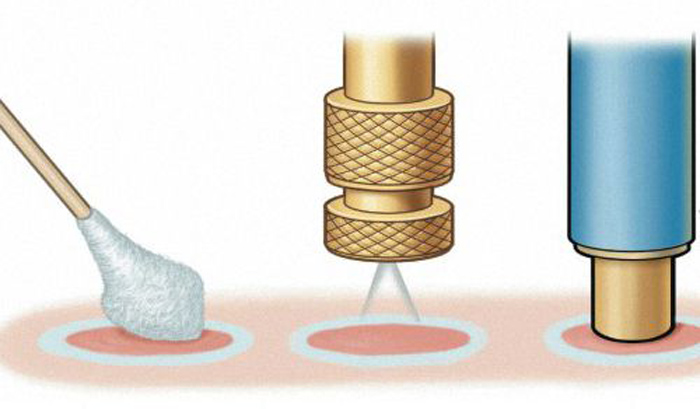
Electrocoagulation is the oldest method, during this procedure a high frequency current is used. The method is used to remove single warts, and most often it is prescribed to women who have already completed their childbearing function. After removal of the growths, the wounds heal for a rather long period, however, relapses with this method of treating genital warts are less common.
Women are recommended Epigen – an antiviral spray that stops the growth of neoplasms and prevents the appearance of new warts. At the same time, it is necessary to take an oral immunomodulatory drug, which will reduce the viral load of the body.
Separately, it must be said about genital warts during pregnancy. Knowing the danger of warts, a woman must undergo a complete examination before conception, and if treatment is required. If the warts are found after the onset of pregnancy, their removal is delayed, as it is dangerous to the health of the unborn child. It is very important to understand that passing through the birth canal, the child can become infected with the virus, so a caesarean section is recommended.
Folk remedies
There are many different remedies for removing genital warts in folk medicine. But not all of them are effective and harmless, so consultation with a doctor about the use of a particular folk recipe is required.
Most often, warts are removed using celandine. Pharmacy tincture or homemade tincture is applied several times a day to the wart, carefully making sure that the product does not get on healthy tissues – celandine is a poisonous plant that can cause severe burns.

Propolis tincture can also be used. It can be used both externally and internally.
Onions and garlic are not in vain famous for their healing properties. The juice of these plants can save a person from the manifestation of a fungal and viral infection. Onion or garlic juice should be used to treat the affected area up to 10 times a day.
Despite the fact that the following recipe is often surprising, it is quite effective in helping to remove warts on any part of the body. 2-3 times a day, it is recommended to apply a piece of banana peel, which is soaked in lemon juice, to the site of the lesion.
Why they are dangerous, complications and prognosis
If vulvar warts are not treated, complications may include:
- violation of the integrity of the neoplasm, which leads to infection and inflammation;
- suppuration of neoplasms;
- phimosis, if the wart is localized on the frenulum of the penis;
- active growth of warts and an increase in the area of the lesion;
- malignant processes.
As for the prognosis, it is relatively favorable. Even after the removal of genital warts, the risk of recurrence and oncology remains.
Prevention measures
The only effective prevention of genital warts is vaccination against the papillomavirus. But it is advisable to receive it before the first sexual contact, because if the virus has already entered the human body, the vaccine will be completely useless.
Also preventive measures are as follows:
- use of barrier contraception;
- exclusion of casual sexual contacts;
- meticulous personal hygiene;
- getting rid of bad habits;
- regular visits to a gynecologist or urologist.
In most cases, the human immune system is able to suppress the activity of the virus in the body, so it is necessary to maintain immunity at its best – lead a healthy and active lifestyle, eat right, and, if necessary, take immunomodulators and vitamin complexes.








К сожалению, если вирус в организме, то чеснок не поможет. Нужно убрать из организма вирус папилломы, мне пока ни таблетки Изоприносин, ни гели, ни мази не помогли. В инете хвалят Аллокин? Кто-нибудь лечился им?