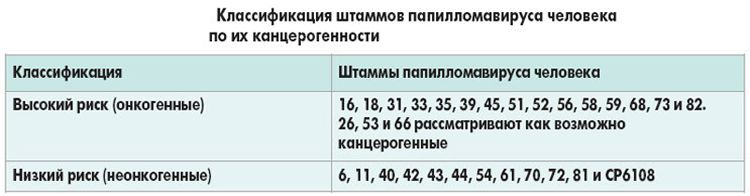
Currently, more than 600 strains of human papillomaviruses have been isolated. Their main difference is the degree of oncogenicity: some types are absolutely safe, others are highly likely to lead to the development of cancer. HPV type 31 is classified as a high oncogenic risk papillomavirus.

Содержание:
- 1 Strain features, how to live, what to do
- 2 What is the danger to the female body?
- 3 Factors provoking pathology
- 4 How it is transmitted and how it manifests itself
- 5 Who is susceptible to infection
- 6 Phases of infection
- 7 Features of development and stage of the disease
- 8 Diagnostics
- 9 papillomavirus therapy
- 10 Prevention
Strain features, how to live, what to do
The virus has a unique DNA structure that cannot be found in any other strain. Its genotype makes the virus carcinogenic. The presence of the pathogen in the body is imperceptible to the patient.
Penetrating into the human body, the type 31 virus almost immediately introduces its genetic material into cells. The tissues undergo serious pathological changes, but there are no symptoms.
Activation of the virus is manifested in the formation of genital warts. In most cases, the reproductive organs are affected. Benign formations are highly likely to degenerate into cancer of the cervix, uterus, ovaries and other organs. In men, papillomas are localized in the anus, penis, scrotum and foreskin.
Men and women are susceptible to infection, and the virus can also be transmitted to the child during the birth process if the mother was infected on or before childbirth.
What is the danger to the female body?
Penetrating into the body of a woman, the virus begins to infect healthy cells. The danger of this type of HPV is that its presence in the body cannot be determined independently. The course of the pathological process is imperceptible to a woman, but changes do occur.
If a woman does not visit a gynecologist regularly, does not take tests, there is a risk of detecting HPV type 31 at a cancerous stage. The virus tends to very quickly provoke cancerous processes in the body, and this is its main danger.
Factors provoking pathology
The human papillomavirus is transmitted mainly through sexual contact, after which it can stay in the body for a long time without showing itself in any way.
At a convenient moment, the virus begins to actively divide, causing pathological processes in the body. The following factors can provoke the activation of papillomavirus:
- Exacerbation of chronic diseases.
- The course of inflammatory processes in the body.
- Development of infections (especially HIV).
- Hypothermia or overheating.
- Weakening of immunity as a result of surgical operations.
- Bad habits (smoking, alcoholism, drug addiction).
- Promiscuous sexual relations.
- Early onset of sexual activity.
- Hereditary predisposition to cancer.
Wrong lifestyle, lack of attention to one’s health, ignoring various unpleasant symptoms, self-medication can also cause the activation of the virus.
How it is transmitted and how it manifests itself
In most cases, the virus is transmitted sexually. It is also possible vertical transmission (from mother to child) and contact-household method (through kissing, using some personal care products, visiting baths, swimming pools, saunas, unhygienic premises in violation of sanitary standards).
During sexual contact, the virus is most commonly transmitted between the ages of 16 and 25 through vaginal, anal, or oral contact.

The virus may not manifest itself for several years or even decades, and under favorable conditions it is activated. The main symptom is the formation of genital warts or soft warts in the genital area and oral cavity.
It is the 31st strain of papillomavirus that provokes Bowen’s disease – the appearance of scaly plaques of reddish or yellow colors, and bonevoid papulosis. Papulosis is characterized by the appearance of soft or warty itchy pigment spots.
In 90% of cases, the virus does not manifest itself in any way and after 2 years a complete self-healing occurs.
Who is susceptible to infection
Everyone is susceptible to infection, but to a greater extent:
- Women aged 16-25 who have begun sexual activity.
- Girls who have begun sexual activity at an early age (up to 16 years).
- Women of young and middle age who do not have a permanent partner.
- Men who are promiscuous.
- Children born to an infected mother.
- Carriers of STIs and chronic diseases of the genital organs.
- People who already have HPV of a different strain in their body.
- All people with various immunodeficiencies infected with HIV.
Phases of infection
For the virus to enter the body of a healthy person, microcracks in the skin or mucous membranes are necessary, which are present in almost all people.
Papillomavirus type 31 penetrates through microcracks into the body during sexual intercourse, petting, using one razor, comb, towel or visiting a public place.
HPV penetrates into the stem cells of the basal layer, which are a constant source of infection of epithelial cells.
Features of development and stage of the disease
Viruses penetrate immature cells of the basal layer at the time of division, the pathogen’s DNA is integrated into the host cells and changes their structure. If a person is already a carrier of another pathogen (another HPV strain, bacterium, fungus), their integration may occur.
While the human immune system is working at full capacity, antibodies are produced that suppress the activity of the virus. Very often, within 6-24 months, the immune system completely rids the body of the pathogen.
If the immune system weakens, the virus begins to actively divide, affecting more and more new cells. The epithelial tissue begins to grow, and this is already becoming obvious: on the skin or mucous membranes (31 strains mainly affect the genital area and oral mucosa), soft warts or genital warts are formed, painless, small, having a different color and structure.

Turning to a doctor immediately after the appearance of papilloma, there is a possibility of suppressing the activity of the virus and reducing the risk of developing malignant tumors.
If the growths are ignored, either the integration of the virus with other pathogens present in the body, or the HPV mutation, as a result of which the malignant process starts, can occur.
The transition of a benign formation to a malignant one is accompanied by unpleasant sensations in the lower abdomen, if we are talking about genital papillomatosis, a sharp weight loss, apathy, fatigue, the appearance of secretions or blood on linen, nausea, lack of appetite and other signs.
The progression of the disease usually occurs within 5 to 30 years, of which 1-3 months is the incubation period. Next, there are stages:
- Asymptomatic course.
- Clinical forms (papillomas, condylomas).
- Subclinical forms (asymptomatic, visible only in the conditions of a medical examination).
- Latent forms (absence of any signs in the presence of virus DNA).
- Cervical intraepithelial neoplasia.
In the future, the disease develops into a cancerous form.
Diagnostics
Below we will consider the most popular methods for diagnosing papilloma type 32.
Pap smear
PAP smear (pap test, smear for oncocytology, cytology of the cervix) allows you to identify atypical cells of the cervix at an early stage.
The analysis is no different from a standard gynecological examination: the doctor carefully, using a special brush, takes a scraping from the walls of the cervix, places it on a glass slide and sends it to the laboratory for microscopic examination.
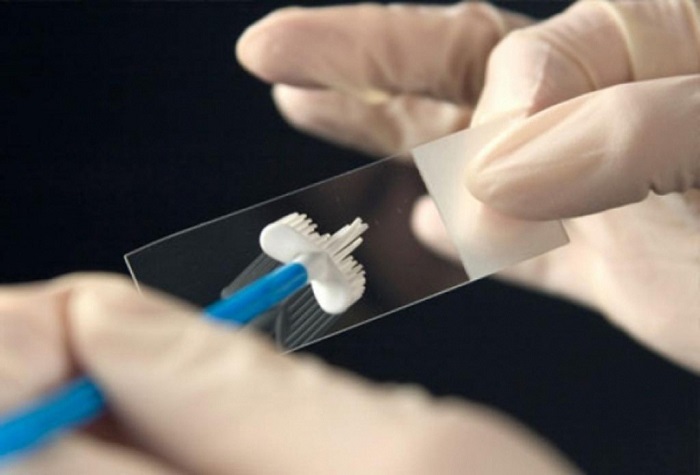
The procedure itself takes no more than 2-3 minutes, and the results are ready in 1-2 weeks (if cervical cancer is suspected, the time for the results to be ready is reduced).
Based on the Pap test alone, the diagnosis is not made: a colposcopy, a blood test and other procedures are required.
Biopsy
A biopsy is prescribed if there is an assumption about the oncological process in the female body. To do this, a small area of damaged cervical tissue is taken and examined under a microscope.
Currently, a biopsy is the most common method for diagnosing HPV, dysplasia, erosion and cervical cancer.
Colposcopy
Colposcopy is a gynecological examination method in which the doctor examines the condition of the cervix using a mirror and a colposcope under high magnification. If the pathological process is started, the doctor will detect tissue growths, bleeding and other signs of erosion or cancer.
As a rule, when lesions are found, a small piece is taken for a biopsy.
papillomavirus therapy
What are the methods of treating HPV in our time and will they help get rid of growths forever?
Conservative therapy
Treatment of HPV type 31 with medication is ineffective, especially if the virus has been in the body for a long time. Such therapy is possible in combination with other methods of treatment.
Conservative elimination of the virus consists in taking immunomodulating and immunostimulating drugs, vitamins, antiviral agents.
If there was one accidental unprotected sexual contact, it is recommended to use the Betadine antiseptic.
During treatment, sex without a condom is prohibited. It is also necessary to study and treat the woman’s sexual partner.
Folk remedies
The use of traditional agents in relation to a virus with a high degree of oncogenicity causes controversy among doctors. Many believe that various compresses and herbal decoctions can only aggravate the situation, since the most delicate skin and genital mucosa can be damaged by them.

Nevertheless, women still continue to use various herbal teas, make compresses and baths. The most popular folk remedies are:
- Compresses from fresh celandine juice.
- Applying freshly cut leaves of Kalanchoe to papillomas on the genitals.
- Consume 1 clove of garlic daily.
- Ingestion of ginseng decoction.
- Phytocollection of horsetail, plantain, nettle, lemon balm, dandelion root and rose hips (3 tablespoons of the mixture pour 800 ml of water, boil, insist and take a glass of infusion half an hour before each meal).
Mechanical removal of growths
Mechanical removal of papilloma is not permissible in all cases and is possible only after a detailed diagnosis. Currently, several methods are used to get rid of papilloma in a medical institution:
- Surgical excision under local or general anesthesia.
- Cryosurgery – freezing with liquid nitrogen.
- Electrocoagulation – the impact on the build-up with an electric current of high frequency.
- laser removal .
Each of these methods has its advantages and disadvantages, and the effectiveness of one or another method of removal and possible risks are discussed in each case individually.
Prevention
There is no 100% protection against the papilloma virus, but preventive measures will help reduce the risk of developing papillomatosis and cancer. These include:
- Abstinence from sexual activity until full puberty (for girls – not earlier than 16-18 years).
- Rejection of bad habits.
- Use of condoms during sex.
- Visiting a gynecologist for preventive examination at least once a year.
- Refusal of promiscuity.
- Commitment to a healthy lifestyle.
- Compliance with personal hygiene measures, use only individual hygiene products and devices (comb, razor, toothbrush).
Currently, HPV vaccination is also popular, but its effectiveness also causes a number of controversies. Many experts recommend vaccinating against papillomavirus during adolescence.
Among the numerous varieties of papillomavirus, HPV type 31 occupies a separate place. It can be asymptomatic in the body, causing various changes in the tissues of the genital organs and cervix.
It has been proven that in 60% of cases, infection occurs during the first sexual contact, so girls should take their health very responsibly. Maintaining a healthy lifestyle and timely access to a doctor significantly reduce the likelihood of infection.







