Unaesthetic skin growths cause maximum discomfort, especially for women. Warts often cover the exposed parts of our body, and this is not the only reason to be concerned about this.
In some cases, a wart is a harbinger of cancer.

Содержание:
- 1 What it is?
- 2 The main differences from other growths on the surface of the skin
- 3 Causes of growth
- 4 Varieties of neoplasms and localization sites
- 5 What is the danger to human health?
- 6 What to do and which doctor to contact when growths appear
- 7 Diagnostic methods
- 8 How to treat growths
- 9 Preventive therapy
What it is?
A wart is usually called a benign nodular formation on the skin. Despite the fact that such a pathology is not inflammatory in nature, warts require mandatory treatment. Otherwise, over time, their number on the skin can increase significantly.
The main differences from other growths on the surface of the skin
You can distinguish a wart from all other skin growths in shape, color, structure and main localization.
Вид нароста Этиология Внешний вид Структура Локализация Бородавка вирусная серо-жёлтая, ближе к телесному цвету; возвышается над кожей, выглядит её частью жёсткая ороговевшая поверхность верхние и нижние конечности; склонна формироваться в «колонии» Родинка наследственность, УФ облучение, иммунодефицит выраженный тёмный пигмент, плоская, выглядит «наклеенной» мягкая без шероховатостей любая часть тела; одиночные Папиллома вирусная телесного цвета, округлая, крепится к коже при помощи ножки мягкая без шероховатостей шея, лицо, пах и подмышки; одиночные
Causes of growth
The appearance of warts on the skin always signals a certain type of human papillomavirus (HPV) parasitizing in the body.
The virus penetrates the epithelium and invades the cell nucleus, where it continues its development and further reproduction.
Infection
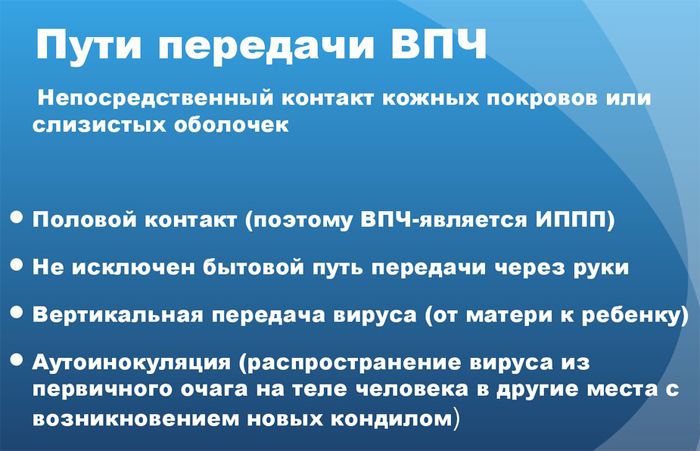
Papillomavirus infection occurs in several ways:
- shared use of household and personal hygiene items;
- by penetration through microcracks and wounds on the skin;
- during a handshake
- when visiting the pool, gyms, saunas, baths;
- in the process of childbirth: from mother to child;
- insufficiently sterilized manicure and pedicure tools;
- genital warts are transmitted sexually .
Provoking factors
In a latent state, HPV can exist in the body for several years or even a lifetime, without manifesting itself symptomatically. But a weakened immune system activates the virus, and this happens under such circumstances:
- avitaminosis;
- diabetes;
- hormonal disorders;
- oncology;
- genetic and chronic diseases;
- psycho-emotional stress;
- physical and psychological overwork;
- meager monotonous food;
- non-compliance with personal hygiene;
- sweating of the feet caused by wearing parka shoes;
- allergic rash;
- alcohol abuse, smoking.
Varieties of neoplasms and localization sites
Depending on the specific type of HPV that provoked the formation of a wart, the growths differ in structure, size and habitual localization.
plantar
They differ from other species in their coarser structure and larger size. The wart is surrounded by a corn-like roller. They are located on the toes, the inside of the foot, a wart on the heel .

The systematic wearing of tight shoes and high-heeled shoes can provoke the development of such a wart. Growing, often begin to cause pain or discomfort when walking.
hanging
Skin formation oval, rounded or irregular in shape. They can be of different colors: from pink and flesh to brown. They occur both singly and in multitudes. In the latter case, from the side, their cluster vaguely resembles a cockscomb.

They form on the neck, face, under the mammary glands, in the armpits, in the groin and even on the scalp. Completely painless, but due to frequent friction on clothing, they can cause discomfort.
filiform
Acrochord is a type of hanging wart. It has an elongated shape and a thin stem. The wart most often retains a flesh color.

Filamentous formations
They tend to unite in a kind of “inflorescence”. Acrochords typically appear in places with the thinnest and most delicate skin: in the armpit, under the breast , on the side of the neck and in the area around the eyes.
flat
They are found mainly on the back of the hand, on the face, knees and legs. Typical for childhood and adolescence.
They look like small nodules of a round or irregular shape with a flesh or yellowish tint. Almost do not rise above the skin. In some cases, they are able to eliminate themselves within a year or several months.

Flat papilloma
Vulgar
The most common form of growth, i.e., the usual round wart with a rough surface. It can occur on any part of the body, but most often on the hand, fingers, face and feet.
They usually form in small clusters. The largest wart in size – the “mother” is located in the center. If it is deleted, all other children can leave on their own.

What is a wart
warts
Anogenital type of warts, better known as genital warts. Able to grow in size fairly quickly. Formations are localized on the skin and mucous membranes of the perianal zone and genital organs.
With further proximal spread, they occur at the entrance to the urethra. The surface of the wart often resembles cauliflower inflorescences. If the mucous membrane of the genital organs with microtraumas, infection with condylomas occurs sexually.

senile
Age keratoma. The wart develops in several stages: from a flat brown-brown spot to a formed skin horn that protrudes significantly above the skin.
They are considered a genetic predisposition and begin to develop slowly after 65 years. May be partly due to frequent exposure to the sun, lack of essential vitamins and oily seborrhea.

What is the danger to human health?
Due to the rapid and erratic cell division that HPV activates, the virus is considered to be oncogenic.
The transformation of a wart into a malignant one can occur 10 or even 20 years after its appearance. This is facilitated by its damage, bleeding, suppuration and changes in color.
The impetus for the manifestation of rebirth can be venereal diseases, alcohol abuse, smoking, a sharp decrease in immunity and obesity.
Flat warts on the cervix are prone to rebirth. A patient with this form of warts should be systematically examined by a gynecologist. At the same time, any injured skin growth is potentially dangerous.
What to do and which doctor to contact when growths appear
In no case should you try to get rid of the wart yourself. Whether it needs to be treated somehow or the wart is completely harmless – only the dermatologist will decide.

Diagnostic methods
During the examination, it is usually not difficult for a dermatologist to determine the type of wart by the following external signs:
- form;
- localization;
- surface: smooth and even or rough rough;
- the presence or absence of a skin pattern on the surface of the growth;
- the presence or absence of pain and itching;
- child warts near the main one;
- thrombosed capillaries on old growths.

In some cases, for completeness of the study, there is a need for histological analysis, examination with a Wood’s lamp and scraping with further PCR diagnostics.
How to treat growths
Effective specific therapy against papillomavirus still does not exist. Treatment in this case is purely symptomatic, but there are several important conditions for its start:
- the wart bleeds, the patient is concerned about severe burning or itching;
- the wart progressively grows and occupies an increasing surface of the skin;
- causes significant discomfort from the cosmetic side;
- the patient is uniquely set to remove the build-up;
- The patient is diagnosed with immunodeficiency.
Medications
Conservative therapy consists of both local treatment of growths and internal administration of antiviral and immunostimulating agents.
Preparations with a necrotizing effect involve external processing. This is oxolinic ointment, Kondimed or Kondilayn, Verrukacid, Solcoderm, lactic acid, Vartek, Viferon or silver nitrate.

For example, to get rid of flat warts , for 3 weeks three times a day you need to take magnesium oxide from 0.15 to 0.25 g. For 1.5 months, the growth is treated with Tretinoin 2 times a day, phonophoresis is performed with interferon ointment .
For the treatment of plantar and common warts, intralesional administration of Bleomycin or Interferon, cauterization with trichloroacetic acid, rubbing colhamic, fluorouracil or interferon ointment into the growth is relevant.
Removal of formations
The most popular and reliable ways to remove warts are listed below.
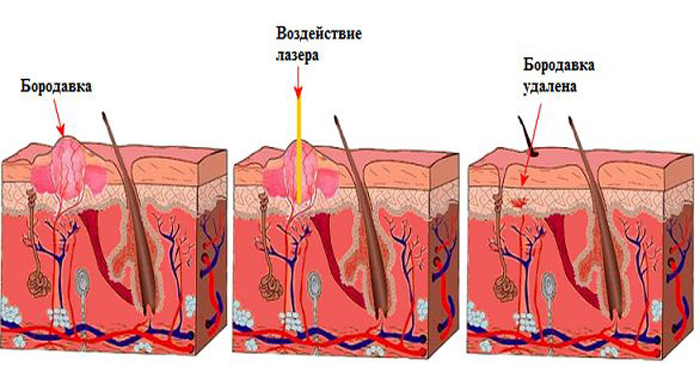
With a laser
Laser therapy allows you to influence not only the surface of the build-up, but also its root. Thanks to this, the wart can be removed the first time.
The growth is removed in layers under local anesthesia. In its place, a slight depression will remain, which will spontaneously level out over the next month.

Healing takes place without complications, does not require special care, and is completely safe for children. It is strongly not recommended to remove the crust formed at the site of the wart.
Thus, you will provoke the appearance of a rather noticeable scar in its place. After one and a half or two weeks, it will fall off on its own.
Getting rid of liquid nitrogen
Under the influence of low temperature, freezing and destruction of tissue occurs at a deep level. The procedure is called cryodestruction and can be performed both in hardware and manually.

The second option increases the risk of damaging the surrounding healthy tissue, but in beauty salons it is used most often. Liquid nitrogen in this case is applied to the wart with a cotton swab.
The growth is frozen for up to 40 seconds. The wart becomes very dense and milky in color. After a few days, a small bubble forms instead, which will completely dry out in 7-10 days.

The crust will fall off on average after 2 weeks, leaving a light pink spot. The procedure usually does not require anesthesia.
Electric cauterization
The wart is destroyed by high-frequency current. The essence of the principle is in cauterization of the base of the growth and the associated adhesion of all the capillaries that are located inside.
The procedure is performed with a coagulator with a heated loop-electrode, which is put on to the very base of the wart and carefully cuts it off. The notch at the site of the build-up is cauterized with a ball nozzle of the electrode.

Excision with a scalpel
The method is relevant for large size and deep rooting of the skin growth, or merging into one whole of several large warts. The operation is performed under local anesthesia.
If necessary, along with a part of healthy tissue, the surgeon cuts out the wart with a scalpel. Excised material often requires histological examination.

After resection, the skin is connected with a silicone absorbable patch or cosmetic suture. The patch will last 2-3 weeks, and stitches can be removed after 7-10 days. The first 14 days after excision, it is desirable to cover the injured area from direct sunlight.
Folk remedies for fighting growths
- Apply a layer of onion to the wart for 2-3 hours until a slight burning sensation occurs.
- Pound lard, onion and vinegar into a pulp and lubricate the wart at night.
- Pour a clove of garlic with vinegar essence for 3 days. At night, apply a cut to the wart. Especially effective for plantar growths.
- Mix garlic, vinegar and flour in equal proportions and lubricate the growths with the resulting slurry.
- Soak lemon slices in vinegar for 14 days. Apply small pieces to the wart until it disappears completely.
- From 2 to 5 times every day, lubricate the wart with ordinary iodine.
- Tie the growth at the very base with a cotton or silk thread pre-soaked in vinegar and leave it like that for a week.
- Tie the wart tightly with a thread and treat it for a week with laundry or tar soap.

Pros and cons of treatment options
The undoubted advantages of any hardware treatment are painlessness, the possibility of deep exposure, the speed and effectiveness of the procedure, the absence of age restrictions, rapid wound healing , and safety against infection.
Treatment with folk methods sometimes takes too long a period of time and never guarantees a 100% cure.
Preventive therapy
Unfortunately, there is no guaranteed protection against HPV. You can protect yourself from the potential development of warts by strictly observing personal hygiene and periodically increasing the level of the immune system.
Always treat any, even minor, cut on the skin with an antiseptic. When working with chemicals, do not forget to wear special gloves. And by all means, avoid sharing personal hygiene products.







